When arthritis is rheumatic
Last month we talked about the more common osteoarthritis and how the disease presents and is best managed. Osteoarthritis (OA) and rheumatoid arthritis (RA) are very different diseasesand are therefore managed quite differently. They are often confused when speaking about sore joints in the patient and general populations.
The cause of RA is not yet fully understood, although doctors do know that an abnormal response of the immune system plays a leading role in the inflammation and joint damage that occurs – the reasons are not known, but can involve genetics, hormones and the environment. Recent research has shown that people with a specific genetic marker called the HLA have a fivefold greater chance of developing rheumatoid arthritis than do people without the marker and this gene controls the immune response in the body.
Researchers continue to investigate other factors that may play a role, including infectious agents such as bacteria or viruses, female hormones (70 percent of people with RA are women), obesity or in response to stressful events.
The 5 features of rheumatoid arthritis
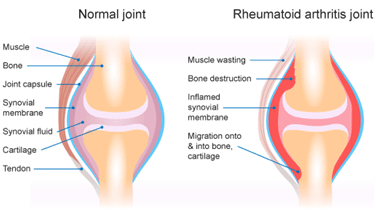
- RA is an auto-immune disease. This kind of condition causes the body's immune system to attack itself. Normally, your immune system makes antibodies that attack bacteria and viruses, helping protect your body against infection. If you have RA, your immune system sends antibodies to the lining of your joints, where instead of attacking harmful bacteria, they attack the tissue surrounding the joint.
- Doctors and medical research haven't really found a cause for RA. There has been a link to people who smoke or have a family history of this disease. It is not yet known what triggers the initial attack. Some theories suggest that an infection or a virus may trigger RA, but none of these theories has been proven.
- RA usually affects the smaller joints, such as those in the hands, feet, neck and wrists. Larger joints such as the hips and knees can also be affected.
- RA is three times more common in women than in men. This may be due to the effects of oestrogen (a female hormone). Research has suggested that oestrogen may be involved in the development and progression of the condition. However, this has not been conclusively proven. Children can also suffer from RA, called Juvenile Arthritis (JA).
- RA is characterised by periods of the disease being either dormant or in a time of 'flare up'. With the joint lining being attacked and all inflamed at these flare up times, there is the presence of hot and swollen joints which are intensely painful to touch and to move. Pain is worst in the morning and can take hours to ease. It actually gets worse with rest and feels better with gentle movement or as the day progresses. RA can also affect the tear ducts, salivary glands the lining of the heart and the lungs, all being very red and sore.
Diagnosing and managing rheumatoid arthritis

In its early stages, RA may resemble other forms of inflammatory arthritis. No single test can confirm RA. To make a proper diagnosis, the rheumatologist will ask questions about personal and family medical history, perform a physical exam and order diagnostic tests. The doctor will examine each joint, looking for tenderness, swelling, warmth and painful or limited movement. The number and pattern of joints affected can also indicate RA, as this type of arthritis tends to affect joints on both sides of the body. This is unlike OA which tends to affect a joint here or there with no particular pattern.
Blood tests are critical to diagnosing RA as inflammation levels and other bio 'markers' can be found in bloods which can be used in addition to the other clinical findings to properly conclude that the arthritis is RA. These include rheumatoid factor (RF) or another anti-body (anti-CPP) which have been found in up to 80% and 70% of those with RA respectively.
Finally, investigations such as Xray, MRI or ultrasounds can assist with diagnosis that can show joint erosion, and narrowing or deformity of the affected joints. These scans are not independently conclusive as there can be the presence of RA in some persons without yet any changes to the joints that would show up on scanning.
Unlike OA, the treatment of RA relies heavily on aggressive drug therapy to stop the inflammatory process to put the disease into an 'inactive' or 'remission' state. The goals of rheumatoid arthritis (RA) treatment are to:
- Stop inflammation (put disease in remission) as early as possible
- Relieve symptoms
- Prevent joint and organ damage
- Improve physical function and overall well-being
- Reduce long-term complications.
Drug therapy initially includes anti-inflammatory for symptomatic relief and slowing of the inflammatory process, steroids and disease-modifying anti-rheumatic drugs, some which are also used to treat some cancers.
Non-pharmacological therapies involve a mix of rest in the highly inflamed periods and gentle exercise, stretches and strengthening to support the affected joints in periods when the disease is less active ad pain levels are lower. This is where your friendly physiotherapist would work with the patient, the rheumatologist, the current phase of the disease (active or in remission) to prescribe a specific exercise program. As with OA, the guidelines for exercise for RA are very similar, however with the RA patient, pain, inflammation and flare-ups are a primary concern. The guidelines are:
- There need to be the right balance between exercise and rest. Too much of the wrong exercise can load up the affected joints more and cause increases in pain, inflammation and long term joint damage. Too much rest and no exercise makes the joints also stiffen and the muscles around to weaken.
- All joints in the human body require synovial fluid and lubrication to stay mobile. This fluid will be secreted by the cells in your joint with the response to movement. So, move it, or lose it (as they say)!
- Too much heavy weight bearing exercise such as jogging, jumping, lifting can over load already painful eroded joints. Preventing repetitive joint loading tasks where possible, including kneeling, squatting or heavy lifting
- Muscular support and strength about the OA joints will make will offer support and shock absorption that would otherwise be transmitted into the painful joint. Good muscle condition is paramount. Pilates could really be a winner here!
Preventing arthritis
Rheumatoid arthritis cannot be prevented as it is an unlucky person who is afflicted with this auto-immune disease. If your joints are painful and there are many afflicted at the same time, referral to a rheumatologist specialised in RA would be recommended.
If you are worried about any joint pain you are having, speak to one of our physiotherapists at The Fix Program.