Is relaxin as good as it sounds?
A woman's body completely transforms during pregnancy, growing and stretching all over in a very short time. Supporting the growing weight requires all sorts of internal reorganising, particularly in the lower back and pelvis. The pelvis eventually becomes elastic enough to allow a baby to pass right through the middle of it – all of this, and more, thanks to the hormone relaxin.
Where does it come from?
Relaxin is produced by the sex organs in both men and women, just like many other hormones. Each gender uses it to do different things, but it gets its name from its role in reshaping a pregnant woman's body. Relaxin production surges within a few days of conception, and the uterus, placenta and breasts start making it too. Its levels are the highest in both the first trimester and at delivery – we'll soon see why!
What does it do?
The increased relaxin directs the body to reconfigure its blood flow – the mother's organs will be working for two, and there is a lot of plumbing involved! By encouraging a widening or a relaxing of specific blood vessels, the body can pump more blood to where it needs to go (your baby via the placenta, the uterus). From there, the relaxin begins to suffuse into the ligaments of the lower back and pelvis, making them far stretchier than before:
The pelvis widens, ready to support the large and sudden increase in abdominal mass. The relaxin continues doing this work, surging once again at delivery – this is, of course, when the ligaments need to be at their absolute stretchiest, giving the baby just enough wiggle and room to escape.
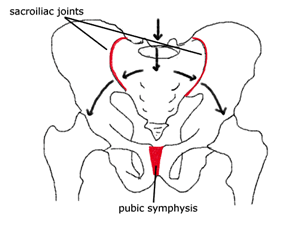
The most affected ligaments are highlighted in red, with the arrows indicating the direction of movement.
So, what's the downside?
Ligaments are usually tight and strong in non-pregnant people, serving to distribute force and weight evenly up and down the body. When they become relaxed and flexible, your muscles have to tighten, working harder to compensate. For pregnant women, this can mean a lot of strain in the pelvis, buttocks and lower back that only gets worse as the baby gets bigger and the ligaments even softer.
What kind of effects does this have?
If the pain is concentrated at the front, it could be what is called pubic symphisis pain (PSP). The ligament responsible is located where your two pubic bones join together – right in the middle, above your genitalia. When it widens, or when one side rises or falls relative to the other, it can become extremely painful and tender to the touch. It is most commonly felt when
- rolling in bed,
- getting in and out of the car,
- climbing stairs
- or when just walking.
If you experience such pain, usually offering compression or stability about the joint may assist reducing pain and improving every day function. Wearing a pelvic stability belt can help reduce stretching in the affected area, while pelvic compression shorts will help the body hold the two halves of your pelvis together. Developing core stability before and during pregnancy will better prepare your supporting musculature – we know that deep abdominal and pelvic floor muscles can offer support and structure about the joint. This preventative strengthening can mean less chance of pain and a reduction of any pain already in this area of the pelvis. This is a big aim of our pregnancy specific classes offered at The Fix Program.
If the pain is on either side of the tailbone, right where your dimples are, it is called sacroiliac joint pain (SIJ). The pelvic bone or ilium (as it usually effects only one side) can move out of good alignment with the tailbone, leaving you with pain in the lower back or down through your buttocks or upper thigh. These joints are usually responsible for smoothly transferring weight from one leg to the other, so the pain is most commonly experienced during activities that involve standing on one leg while lifting the other, including
- walking,
- standing up from sitting,
- rolling and standing up from bed,
- or even getting dressed.
Fortunately, the treatment for any of these symptoms is the same as for pubic symphisis pain. This will include wearing pelvic compression garments, pregnancy-specific core stability exercises and stretches, and hands-on physiotherapy treatment.
Do the effects last?
The good news is that your ligaments will likely return to normal once the relaxin returns to its normal levels and you are no longer weight-bearing for two. Of those that experience either type of pain during their pregnancy, four out of five women have their discomfort spontaneously resolve within three months after the birth. For the unlucky Ms. Five, there is a lot understood about the pain and many ways that the Fix physiotherapists can help you out!
Relaxin is an amazing part of the incredible transformation of pregnancy, playing an essential role in preparing a woman's body for the task of sustaining and delivering a new life. These changes might be challenging or painful for your body, which is why the Fix team will be ready to help you before, during and after the arrival of your new baby.